Visual Development and Eye Examinations for Children with Additional Support Needs
Presented on Monday 1 February 2010
J Margaret Woodhouse
School of Optometry &
Vision Sciences
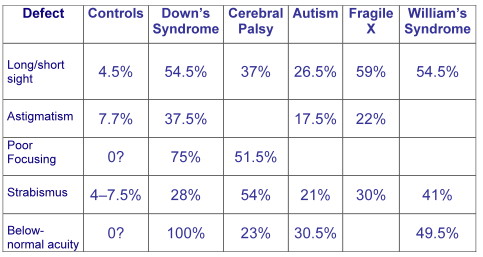
Prevalence of visual defects
Refractive errors
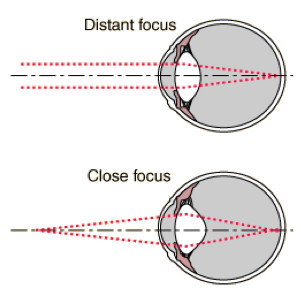
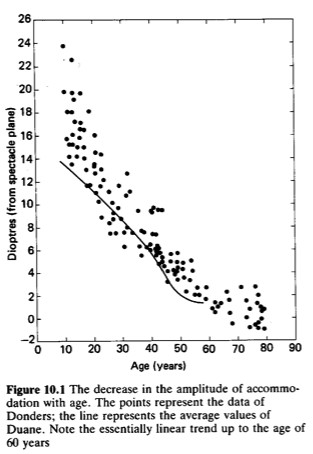
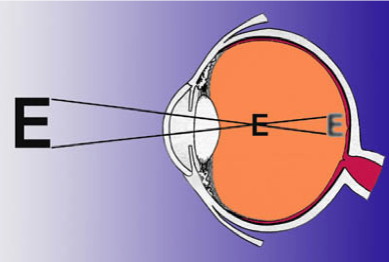
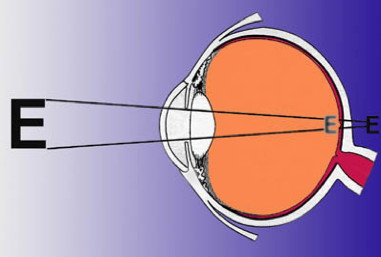
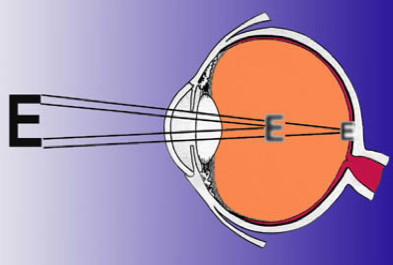
Accommodation - focusing for near
Accommodation reduces with age
Short-sight (myopia)
A short-sighted child
- Lenses to correct myopia (short-sight) are negative eg; -5.00D, -7.50D
- Will have clear vision at near and blurred vision at distance
- Will need to wear glasses for distance eg; watching television and looking at the board
- May choose to wear glasses all the time
- May use eyes 'natural magnification' by removing specs for near
Long-sight (hypermetropia)
A long-sighted child
- Lenses to correct hypermetropia (long-sight) are positive eg; + 2.25D, +6.75D
- Vision will be clearer at distance and more blurred or uncomfortable vision at near.
- Long-sighted children can often accommodate or focus to see clearly without their glasses but will probably not be able to sustain this for long.
- Extent of blur or discomfort will depend on age as well as amount of long-sight.
- May need to wear glasses for near
- May need to wear glasses all the time
Astigmatism
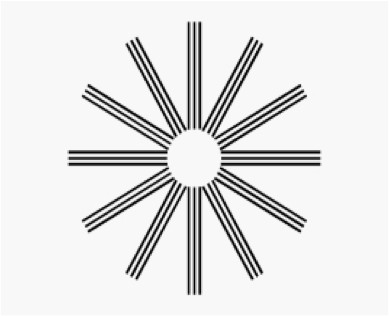
A child with astigmatism
- The astigmatic (cylindrical) component of the lens is the second figure
of the prescription, and the direction of the astigmatism the third part
eg; -1.00 / +0.50 x 90
+3.50 / -1.25 x 45 - Will have blurred vision at all distances.
- May need to wear glasses for both distance and near
- May find adjusting to the glasses very difficult
In general, if the second figure is small compared to the first, the
important aspect is myopia or hypermetropia
-6.50 / + 1.75 x 30 means
myopia
+4.50 / + 0.75 x 10 means hypermetropia
If the second figure is large compared to the first, astigmatism is
the most important aspect
+1.50 / - 4.25 x 175 means astigmatism;
Lenses to correct myopia minify the eyes, while lenses to correct hypermetropia magnify
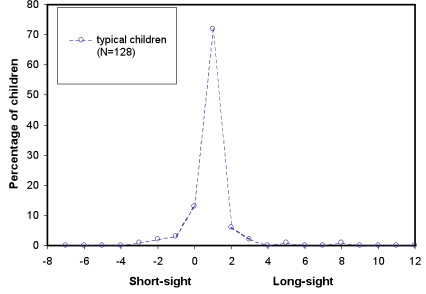
Typical children
Typical school-age children (4-18 years)
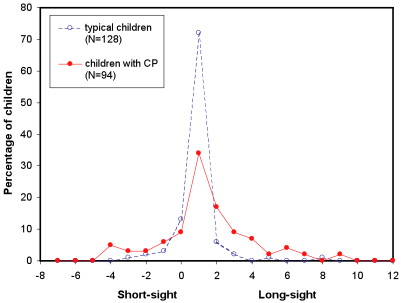
Children with cerebral palsy (Julie McClelland)
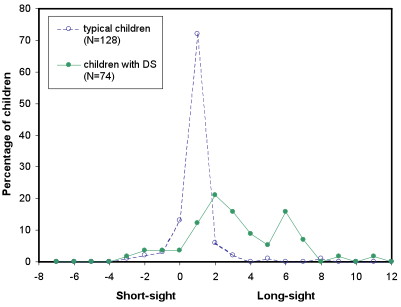
Children with Down's Syndrome
Children with visual impairment
Du et al. (2005) Retrospective Analysis of Refractive Errors in Children
with Visual Impairment. Optometry & Vision Science, 82, 807-816
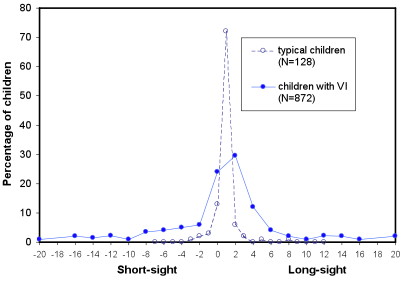
Children with Disabilities
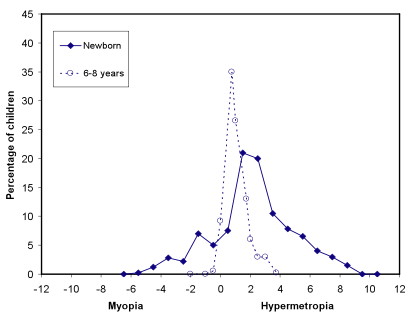
- Probably have the same distribution of refractive errors at birth as typical children
- But are unlikely to outgrow infant errors
- So may need glasses earlier than an ordinary child
What would make us suspect refractive error?
- Short-sight
- Getting very close to things
- Screwing eyes up to see at distance
- Lack of interest at distance - Long-sight
- Getting very close to things
- Lack of interest in near tasks - Astigmatism
- Getting very close to things
Usually, it is NOT possible to spot a refractive error in a child - all children should have an examination
Children learn at near
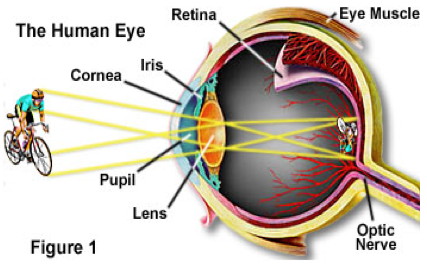
Accommodation - near focusing

Typical pre-school children focus accurately
Typical older adults struggle to focus
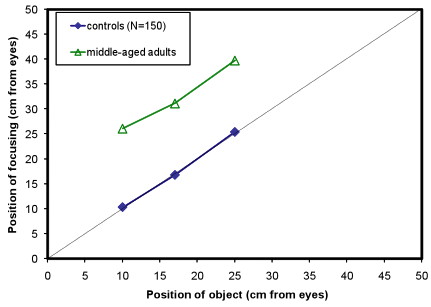
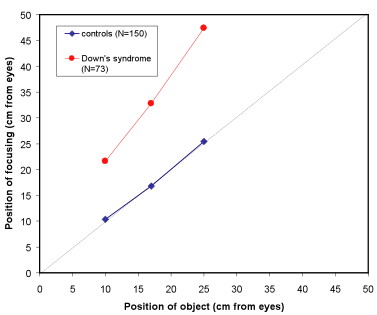
Children with Down's Syndrome
Children with Cerebral palsy
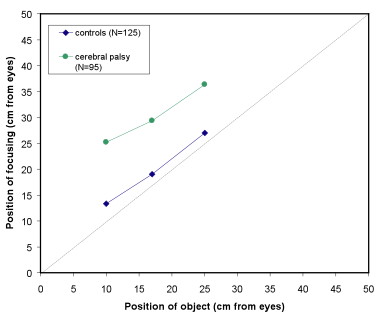
Children with disabilities
- Are likely to have difficulties with accommodation
- May not be able to overcome long-sight (hypermetropia) with the same ease as typical children
- So may need glasses for smaller amounts of long-sight than an ordinary child
- Among children with DS, 76% have poor focusing for near targets
- Among children with CP, 58% have poor focusing for near targets (JF McClelland, J Parkes, N Hill, AJ Jackson, KJ Saunders IOVS, 2006: 47; 1824-1830)
- Children have a focusing error even when they wear glasses for long or short-sight
Near tasks are blurred for most children
What would make us suspect poor accommodation?
- Bringing near tasks very close
- Lack of interest in near tasks, compared to distance
- Bringing head back if objects get too close
Usually, it is NOT possible to spot poor accommodation in a child - all children should have an examination
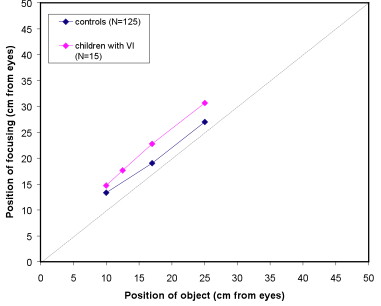
Children with visual impairment
replotted from Leat and Mohr., IOVS, 2007.
What would make us suspect poor accommodation?
In CP, using patches for dribbling
- The patches contain hyoscine, which is a cycloplegic, a similar substance to that used to paralyse accommodation during eye tests
- Paediatricians may not know that hyoscine is a cycloplegic
- Any child using patches should have an eye exam
DS bifocal spectacle trial
- Two groups (17 pairs of children; all of whom under-accommodate)
- matched for :
- age
- cognitive ability
- type of school
- members of the cohort /new recruits
- type of refractive error
- current use of spectacles
- Bifocal group - given specs with a +2.50D add (for use in school only) and had single vision specs for home
- Control group - had new 'single vision' specs for school use and kept their current specs at home
Results
- Excellent co-operation from all schools, teachers and classroom aides
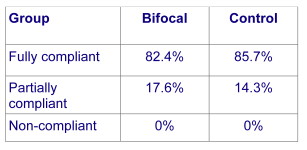
- Positive response from children in both groups to new glasses, and compliance good
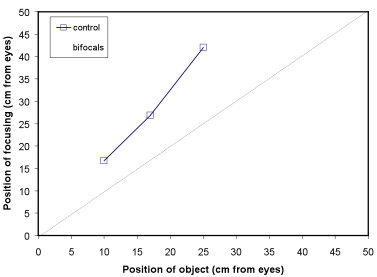
Accommodation
At the outset there was no difference in the accommodation between the two groups (p=0.851)
- control group: mean accommodative deficit = 3.37D ± 1.31
- bifocal group: mean accommodative deficit = 3.44D ± 1.07
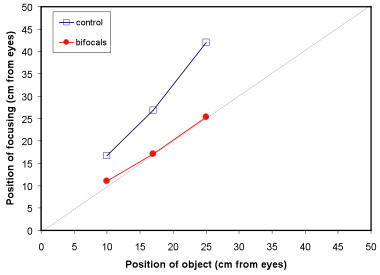
Outcomes of trial
- Children in the bifocal group accommodated more accurately
(Stewart, R E, Woodhouse, J M & Trojanowska, L D (2005) Ophthalmic and Physiological Optics 25 (6), 514-522) - Teachers reported better concentration and writing skills in the children wearing bifocals
- Recent study from Canadian group shows significant
improvement in literacy and visual perceptual skills with bifocals
(Nandakumar and Leat, ARVO abstract 2009. E-3970)
Bifocal wear
- The children use their bifocals very successfully
- We begin with bifocals for school use only, but most children choose to wear their bifocals full-time
- Even (the few) children who are reluctant to wear ordinary specs will wear bifocals happily
Ethan – went into bifocals aged 3 yrs 9 months: email from Mum
Just thought I'd let you know that he took to the bifocals straight away and hasn't put his old glasses back on since wearing them.
Just this morning his key worker at pre school asked me if I'd noticed a difference in Ethan since he's been wearing his bifocals - steadier on his feet, better communication and attention when looking at flash cards and so on. It's nice that someone else has noticed too.
Also, I know I mentioned to you that I was worried about his peripheral vision when we visited because he only seemed to look at 1 out of 4 words on a matching board when we were practising reading. I think it's because he had to try so hard to focus that he could only look at 1 at a time. Now he looks at the whole board and understands better what I'm asking him to do!
Prescribing guidelines
- We used straight-topped D-28 bifocals, fitted with the segment top at, or just below, pupil centre. The fit is critical.
- Bifocals may be temporary – ONE THIRD of children begin to accommodate accurately through the distance part of the lens and can return to single vision lenses
Children with cerebral palsy
- The Coleraine study showed that children benefit from near corrections
- Report from Glasgow Caledonian demonstrates the successful use of
varifocals.
(Ross LM, Heron G, Mackie R, McWilliam R, Dutton GN (2000) Developmental Medicine & Child Neurology 42(10):701-3) - Poor head and eye movement control MUST be taken into account when considering near corrections
Wearing glasses
Children with disabilities may have differently shaped faces to 'ordinary' children
- Children with cerebral palsy may have poor head control that means glasses slip or are knocked around by the head support
- Because of limited mobility and hand-eye co-ordination, children may find adapting to lenses difficult
There are two reasons to wear glasses and LOTS of reasons to reject glasses
- Glasses make the world appear clearer
- To the child, this means that things look 'different'
- The lenses magnify or minify and distances are difficult to judge
- All lenses have distortions - the stronger the prescription, the greater the distortions
- 2.Glasses reduce the effort to see clearly and may reduce a squint
- To the child the glasses may make no visible difference
Encouraging a reluctant child
- Avoid curl sides and sports bands
- Know what the glasses are for and when the child will get benefit
- Pick a favourite activity with undivided attention - this is going to be 'spec wearing time'
- Put glasses on and start the activity
- If your child takes the glasses off, end the activity without comment
- Gradually build up wearing time - don't worry if it takes weeks or even months
- DO NOT TURN IT INTO A BATTLE!
Visual Acuity - letters: Logmar Crowded test (Keeler)
Visual Acuity - pictures: Kay Pictures; Lea symbols (Insight)
Visual Acuity - preferential looking: Cardiff test (www.cardiffacuity.co.uk); Teller Acuity Cards; Keeler Acuity cards
Contrast sensitivity - preferential looking: Hiding Heidi; Cardiff Contrast Test
What would make us suspect acuity or contrast problems?
- Poor visual acuity
- Getting close to objects
- Inability to see detail at distance and/or near
- Lack of interest in detailed tasks
- Poor contrast sensitivity
- Vision is variable (depending on contrast of task)
- Inability to write on the line
- More difficulty with pencil than pen
Behavioural acuity
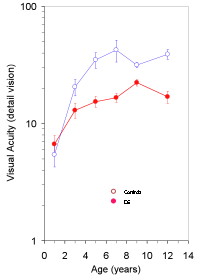
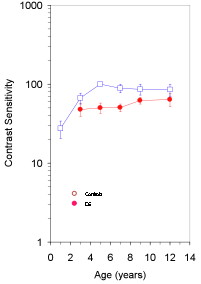
Behavioural contrast sensitivity
Visual Evoked Potentials - VEPs
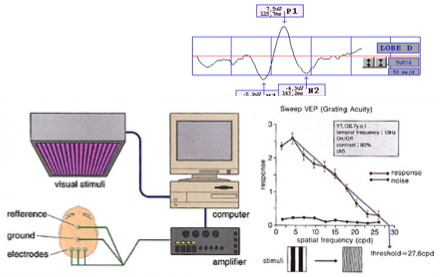
VEP acuity
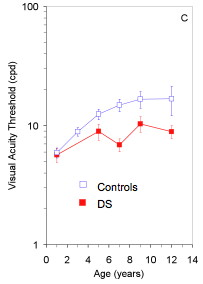
VEP contrast sensitivity
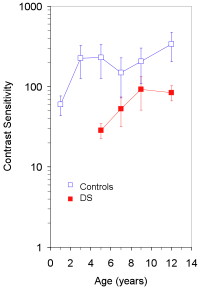
- Children with Down's syndrome have poorer vision than their peers
- This applies to children with no other eye defects, and to children wearing their glasses
Children with cerebral palsy
- May have poor vision associated with CVI;
- Vision can range from normal to no light perception
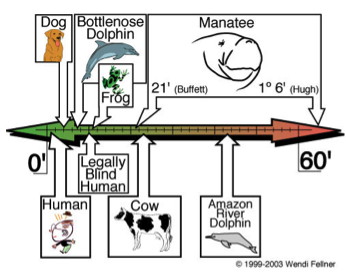
Visual acuity - what do the numbers mean?
- Acuity given by fraction; top figure is the subject's viewing distance, bottom figure is the distance at which 'normal' could resolve detail
- Normal is 6/6
- 6/24 is four times poorer than 'normal'; letters need to be four times closer or four times larger
- In theory, fraction can be treated as real: 6/24 = 3/1 and 3/60 = 6/120
- Number of letters on each line is different
- Spacing of letters on each line is different (relative to letter size)
- Task is different on each line, so 6/24 is NOT the same as 3/12
- Step sizes are arbitrary, so 'acuity improved by two lines' is meaningless
Bailey-Lovie Chart
- Number of letters on each line is the same
- Spacing of letters on each line is the same (relative to letter size)
- Task is the same on each line, so 6/24 is now the same as 3/12
- Step sizes are equal throughout the chart
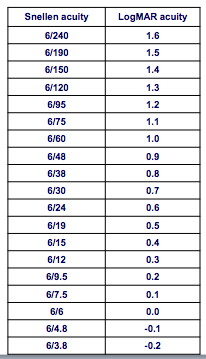
LogMAR Acuity
- Log (to base 10) of the Minimum Angle of Resolution
- 6/60 has MAR of 10 minutes of arc, so LogMAR is Log(10) = 1
- Each line differs from the next by 0.1
- Five letters on each line; each letter scores 0.025
- 6/6 is LogMAR 0, so visual acuity is zero!
- Lower lines (that is, better acuity) have negative scores!
Visual Acuity (VA)
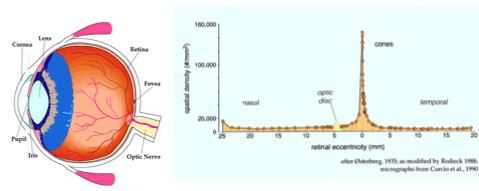
Visual field defects
- Not a characteristic of Down's syndrome
- May occur in cerebral palsy, associated with the site of brain injury
- We all have a blind spot, of which we are NOT AWARE
- A child with a visual field defect WILL NOT KNOW it
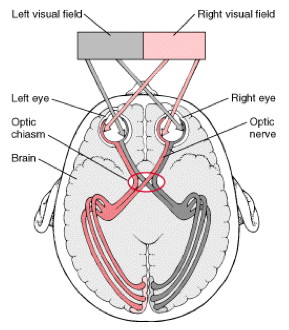
- The right visual cortex represents left visual field and vice versa.
- Defects affecting only the right or left field in both eyes are possible – hemianopia
- One study suggested 75% of children with hemiplegia had hemianopic field defects.
- The lower visual cortex represents upper visual field and vice versa...
- Defects affecting only the upper (uncommon) or lower field (more common) are possible
What would make us suspect visual field defect?
- Mobility problems
- Bumping into or tripping over objects
- Failure to respond to approach from one side
- Surprise or distress if approached from one side
- Extreme difficulty on steps or stairs (lower field defect)
Additional visual / ocular defects in children with Down's syndrome and cerebral palsy
- Refractive errors (60%)
- Poor accommodation (80%)
- Reduced visual acuity and contrast sensitivity (100%)
- Squint
- Nystagmus
- Blepharitis
- Cataracts (8-13%)
- Keratoconus (15%)
- Poor eye movement control
- Cerebral visual impairment
Squint (strabismus) - 25% DS, 54% CP
- Can be associated with any (or no) refractive error
- Is often alternating in DS and CP (alternation is rare in ordinary children) and vision is equal R+L
- Children with CP sometimes use different eyes for different directions of gaze
- In a consistent squint, the image from the non-fixing eye is suppressed
- If a squint is constant in one eye, the nerve pathways from that eye fail to develop fully and amblyopia (lazy eye) results
- Patching reverses the competition and improves acuity in the open eye, but does NOT correct the squint
Nystagmus – 15% in DS, similar in CP?
- Regular 'wobble' of the eyes
- Associated with visual impairment, as with typical children
- Associated with abnormal head posture (null point of nystagmus), as with typical children
- Needs the same support in children with DS and CP as in typical children
Blepharitis - up to 50% in DS
Responds to lid hygiene measures
- Baby shampoo on a clean finger
- Scrub the lid edges every night
Cataract
- Congenital slightly more common in DS and CP than typical infants
- Detected at neonatal checks
- 'Senile' cataracts occur decades earlier than general population
- Cause glare so main feature is difficulty when light is towards the subject
- Reduce contrast perception, very variable vision depending on the background
- Treatment is the same as general population, surgical removal with implant
Cataract extraction

Cataract removed and replaced with plastic implant
Keratoconus – 15% in DS
- Growth of the cornea into conical shape
- Onset teens
- Can stabilise or progress
- Causes increase in myopia (short-sight)
- Not correctable with glasses
- Distorted vision leading to visual impairment
- Correctable, as in general population, with contact lenses
- If progressive can cause corneal scarring
- Late stage treated with corneal graft
Diagnosis of keratoconus in DS
- Cornea becomes thinner and more curved
- People with DS have thinner, more curved corneas to begin with
- Early diagnosis is difficult, but until recently, not important
- Collagen cross-linkage therapy can halt progression
- MUST be carried out at very early stage
Eye movement difficulties
- Problems in making accurate eye movements, or sustaining an eye position
- Distinguish this from nystagmus – the two conditions are quite separate, but can occasionally occur together
- Estimated prevalence of 25% in CP?
What are eye movements for?
- To allow 'best vision' of the object of interest
- To allow localisation of objects
- To 'stabilise' the visual world
- For social interaction
- To keep both eyes aligned
What are the consequences of being unable to make or sustain accurate eye movements?
- Difficulty in concentrating and learning?
- Poor spatial awareness?
- An unstable world?
- Limited social development?
- Double vision?
Poor eye movement control must constitute a severe visual impairment.
Poor eye movement control complicates our assessment of a child's potential vision.
Poor eye movement control limits a child's ability to adapt to
spectacles?
Spectacle lenses
- produce distortions
- cause magnification / minification, that is, distances become difficult to judge
- change the apparent position of objects
Adaptation experiments (1960's): Only subjects allowed full control of hand and body movements adapted to the spectacles.
Children with cerebral palsy may find it much more difficult to adapt to spectacle lenses if they cannot move freely
Visual perceptual deficits and cerebral visual impairment (CVI)
(consult Gordon Dutton or Andrew Blaikie)
- Condition in which vision is disturbed, but the eyes appear fully healthy
- Can range from minor problems in visual interpretation to no light perception
- Reasonably common in CP
- May occur in DS – watch this space!
Thanks to: all of the children who take part in our studies, and their families
woodhouse@cf.ac.uk
